More Information
Submitted: November 30, 2020 | Approved: December 19, 2020 | Published: December 21, 2020
How to cite this article: Ghosh PK, Mollah MMH, Chowdhury AA, Alam N, Harun GD. Hypertension and sex related differences in mortality of COVID-19 infection: A systematic review and Meta-analysis. Arch Biotechnol Biomed. 2020; 4: 037-043.
DOI: 10.29328/journal.abb.1001020
Copyright License: © 2020 Ghosh PK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hypertension; COVID-19; Systematic review; Meta-analysis; Mortality
Hypertension and sex related differences in mortality of COVID-19 infection: A systematic review and Meta-analysis
Probir Kumar Ghosh1*, Mohammad Manir Hossain Mollah2, ABM Alauddin Chowdhury3, Nazmul Alam2 and Golam Dostogir Harun3
1Bridge of Community Development Foundation (BCDF), Dhaka, Bangladesh
2Asian University for Women, 20/H M. M. Ali Road, Chittagong-4000, Bangladesh
3Department of Public Health, Daffodil International University, Mirpur Road, Sukrabad, Dhaka-1207, Bangladesh
*Address for Correspondence: Probir Kumar Ghosh, MSc, Statistical Consultant, 98/2 Lake Circus Kalabagan, (Ground Floor), Dhanmondi, Dhaka-1205, Bangladesh, Tel: +8801712-047987; Fax: +88029809415; Email: [email protected]; [email protected]
Background: Hypertension is the leading cause of cardiovascular diseases and premature deaths. Hypertension plays a striking role in mortality and morbidity in case of Coronavirus Disease 2019 (COVID-19) infection; however, numerous studies have reported contradictory findings.
Objective: To assess the relationship of hypertensive disease and mortality of COVID-19 infection and to assess the sex and age differentials on the association.
Methods: We have conducted a systematic review of published literatures that identified the relationship between hypertension and mortality of COVID-19 infections. Nineteen articles were selected following structured inclusion and exclusion criteria for systematic review and analyses. A total of 21,684 hospital admitted COVID-19 patients were included in this review and meta-analysis from 19 studies. The studies covered the six months of the pandemic from December 2019 to May 2020.
Results: In the pooled analysis, the median age of patients was 58 years, and the proportion of male patients was 58.8%. In contrast, we estimated 33.26% of hypertensive and 19.16% of diabetes mellitus patients in the studies. Hypertension was found to be associated with COVID-19 mortality (“Risk ratio (RR) = 1.45, [95% confidence interval (CI): 1.35 - 1.55]; I2 = 77.1%, p - value < 0.001”). The association in the meta-regression was affected by sex (p - value = 0.050). The association was found to be stronger in the studies with males ≥ 55% and age ≥ 55 years (“RR = 1.65, [95% CI: 1.52 - 1.78]; I2 = 77.1%, p - value < 0.001”) compared to male < 55% or age < 55 years (“RR = 1.11, [95% CI: 0.94 - 1.28]; I2 = 72.2%, p - value < 0.001”).
Conclusion: Hypertension was significantly strong associated with COVID-19 mortality which may account for the contradiction in the many studies. The association between hypertension and mortality was affected by sex and there were significantly higher fatalities among older male patients.
The Coronavirus Disease 2019 (COVID-19) outbreak initially emerged in the early in December 2019 in Wuhan city, Hubei province, China [1]. It was declared a pandemic on 12 March 2020 by the World Health Organization (WHO) [2]. To date, this disease has spread to all five continents and has caused a “Public Health Emergency of International Concern (PHEIC) since 30 January 2020” [3]. As of early August 2020, it has already infected more than 20 million people along with more than 0.7 million deaths. Among them, 99% of cases were mild, 72.50% cases which had an outcome and 5% of fatalities have occurred in 14.50 million known outcomes [4], with deaths rapidly emerging around the globe. Determining the potential factors related to increased mortalityin COVID-19 patients is required for competent resource allocation during the pandemic period, especially in the low-middle income countries.
The burden of chronic diseases has rapidly emerged and causes 41 million deaths each year around the world, in which cardiovascular diseases account for 17.9 million deaths [5]. Hypertension is one of the most severe medical conditions which increases the risk of cardiovascular diseases. Highest prevalence of this condition was observed among COVID-19 patients, followed by other comorbidities [6]. Globally, 1.13 billion people have hypertension and low-middle income countries account for 75% of the total hypertensive patients [7]. Hypertension also causes cognitive impairment in two-thirds of elderly people [8,9]. In an influenza pandemic, older men were more likely to have a severe outcome [10]. Previous studies have shown that virally infected advanced age men with other co-morbidities suffered from weak immune function, however uncertain, may increase susceptibility and mortality of COVID-19 infection [11–13]. Hence hypertension is an important contributor to COVID-19 mortality in relation to age and, and is consistent in different countries worldwide. We aimed to explore the relationship between hypertension disease and mortality due to COVID-19 infection and to assess the sex and age influence on the relationship.
Eligibility criteria
We enrolled all the studies which included COVID-19 infection with hypertension disease, mortality and survival. The original research articles with sample size > 50 hospital admitted patients published in English language were included.
Search strategy and study selection
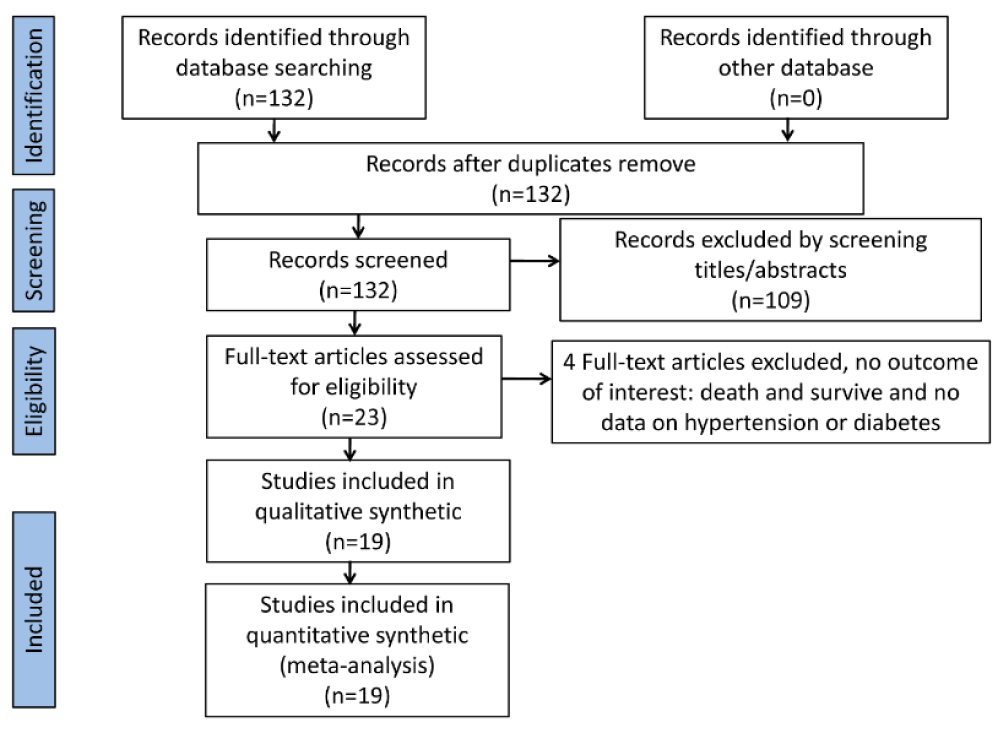
We carried out a comprehensive systematic peer-reviewed literature search by using PubMed, SCOPUS, EuroePMC and Google Scholar databases with the terms: “COVID-19” OR “SARS-CoV-2” AND (“Comorbidities” OR “hypertension”). We removed the replicas of the extracted articles. Two authors (AI and PKG) screened for relevant information in the abstracts of the remaining literature. Based on the eligibility criteria, we examined the full text of selected articles. We completed the article extraction on 31 July 2020followingthe guideline of “Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA)” [14] (Figure 1).
Figure 1: PRISMA flowchart.
Quality assessment of the studies: Quality of the studies included for final review was also assessed in terms of study size, sample selection methods and measurement of study outcomes. The studies were considered poor in quality if they have small sample size, non-random individuals and study outcomes were not measured objectively, moderate quality and better quality studies are those who used large sample, used randomization in patients section, and study outcomes were measured objectively.
Data extraction
Two independent authors (AI and PKG) extracted the 19 studies. We used standardized forms that included author, year, study design, sample size, age, sex, hypertension, diabetes and death of COVID-19 patients. The outcome of interest was mortality due to COVID-19 infection.
Statistical analysis
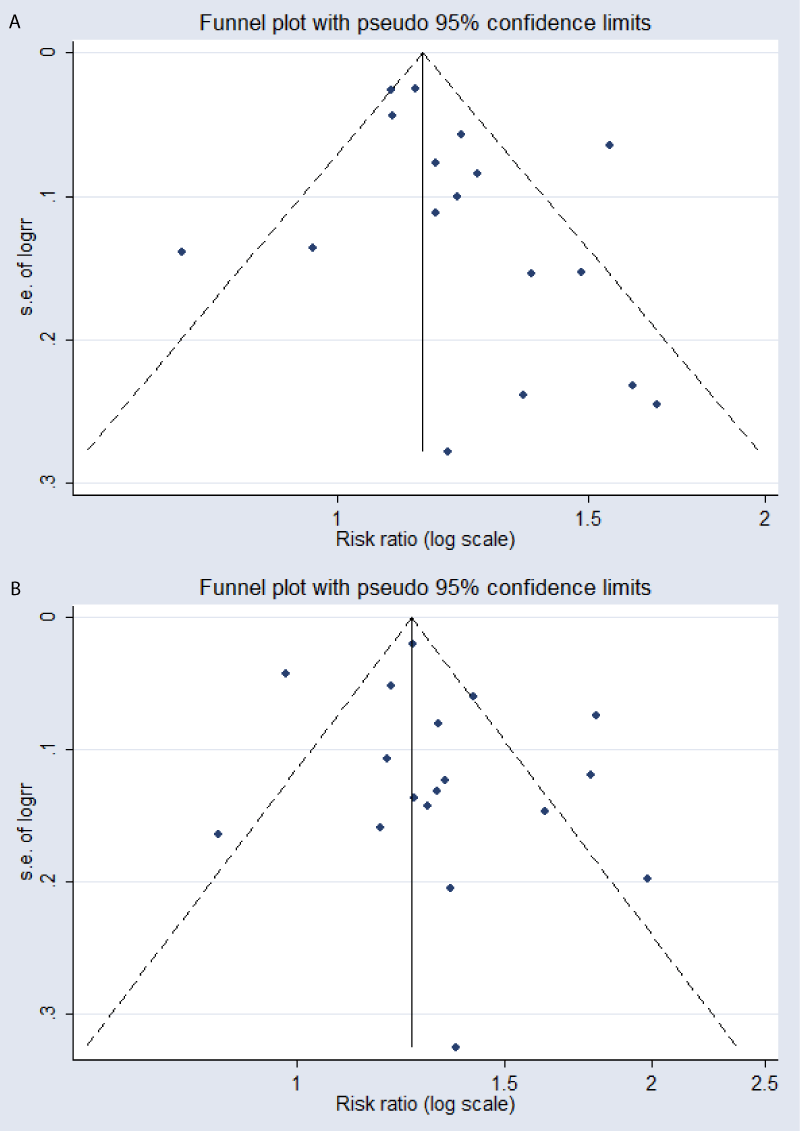
We performed Mantel-Haenszel formula to estimate the effect in risk ratio (RRs) with 95% confidence interval (95% CI) and performed Random-effects model to account for inter-study variability. All p-values in this study were two-tailed and statistical significance was set at ≤ 0.05. Meta-regression was performed to examine the influence of covariates on the RR. We conducted further subgroup analysis to assess the more influential group in the magnitude of RR based on median age and average proportion of hypertension in the studies. To evaluate the small-study effects, we performed a regression-based Egger’s test. We performed Funnel-plot analysis to identify the qualitative bias in the publication.
Characteristics of the included studies
While we extracted an initial 132 studies, there were no duplicate records and we excluded 109 studies after screening the abstracts. The remaining 23 studies were eligible for full-text screening. We eliminated four studies because of no available data on sex, age, hypertension or diabetes. Finally, we included 19 articles for qualitative synthesis and meta-analysis (Figure 1) (Table 1).
| Table 1: Characteristics in the included studies. | ||||||||
| Study | Setting | Duration | Sample size | Study Design | Median/Mean age | Male (%) |
Diabetes Mellitus (%) |
Hypertension (%) |
| Lang W, et al. [33] | Renmin Hospital, Wuhan, China | 1 Jan to 5 Mar 2020 | 339 | Observational Retrospective |
71 | 49.00 | 16.00 | 40.80 |
| James, et al. [34] | King’s college and Prince university hospital, London | 1 Mar to 22 April 2020 | 1157 | Observational Retrospective |
71 | 57.60 | 35.30 | 52.90 |
| Hu K, et al. [35] | Yangtze River Shipping General hospital, Wuhan, China | Jan to Mar 2020 | 105 | Observational Retrospective |
58 | 62.90 | 0.00 | 17.10 |
| Chen L, et al. [36] | Union, Central, General and Jin-Yin-Tan Hospital, Wuhan, China | 26 Jan to 4 April | 1651 | Observational Retrospective |
59 | 50.00 | 14.00 | 31.0 |
| Ali, et al. [37] | Fars, Iran | 18 Feb to 19 Mar 2020 | 440 | Observational Retrospective |
46.5 | 56.40 | 7.50 | 7.95 |
| Pablo, et al. [38] | Three hospital, London | 25 Feb to 4 April 2020 | 614 | Observational Retrospective |
69 | 62.00 | 27.50 | 35.00 |
| Riccardo, et al. [17] | Civil hospitals of Brescia, Lombardy, Italy | 4 Mar to 25 Mar | 99 | Observational Retrospective |
67 | 81.00 | 31.00 | 64.00 |
| Chao G, et al. [39] | Zhongnan hospital, Wuhan, China | 5 Feb to 15 Mar 2020 | 2877 | Observational Retrospective |
60 | 51.10 | 13.50 | 29.50 |
| Zhou, et al. [18] | Jinyintan and Pulmonary hospital, Wuhan, China | Up to 31 Jan 2020 | 191 | Observational Retrospective |
56 | 62.00 | 19.00 | 30.00 |
| Giacomo, et al. [40] | Lombardy, Italy | 20 Feb to 30 May 2020 | 3988 | Observational Retrospective |
63 | 79.90 | 12.89 | 41.20 |
| Chaomin, et al. [19] | Jinyintan hospital, Wuhan, China | 25 Dec 2019 to 26 Jan 2020 | 201 | Observational Retrospective |
51 | 63.70 | 10.90 | 19.40 |
| Mandeep, et al. [41] | Asia, Europe and North American hospital | 20 Dec 2019 to 15 Mar 15 2020 | 8910 | Observational Retrospective |
52 | 59.90 | 14.28 | 26.30 |
| Bai T, et al. [6] | Jinyintan hospital, Wuhan, China | 26 Dec 2019 to 31Jan 2020 | 127 | Observational Retrospective |
55 | 63.00 | 11.80 | 28.30 |
| Cao J, et al. [39] | Huoshenshan hospital, Wuhan, China | 3 Jan to 1 Feb 2020 | 102 | Observational Retrospective |
54 | 52.00 | 10.80 | 27.50 |
| Lu Z, et al. [42] | Seventh hospital, Wuhan, China | 1 Jan to 15 Feb 2020 | 123 | Observational Retrospective |
63 | 49.60 | 11.40 | 33.30 |
| Chen T, et al. [32] | Zhongnan hospital, Wuhan, China | 1 Jan to 10 Feb 2020 | 55 | Observational Retrospective |
74 | 61.80 | 30.90 | 38.20 |
| Lin Fu, et al. [20] | Union hospital of Huazhong Wuhan, China | 1 Jan to 30 Jan 2020 | 200 | Observational Retrospective |
55 | 49.30 | 68.20 | 51.50 |
| Kaiyan L, et al. [21] | Tongji hospital, Wuhan, China | as of Mar 20 | 102 | Observational Retrospective |
57 | 58.00 | 15.00 | 30.00 |
| Xia L, et al. [43] | Eastern campus of Renmin hospital, Wuhan, China | as of Feb 25 | 403 | Observational Retrospective |
56 | 47.90 | 14.10 | 28.00 |
The selected studies covered the six months of the pandemic from December 2019 to May 2020 and included 21,684 patients. In the pooled analysis, the median age of patients was 58 years, and the proportion of male patients was 58.8%. In contrast, we estimated 33.26% of hypertensive and 19.16% of diabetes mellitus patients in the studies.
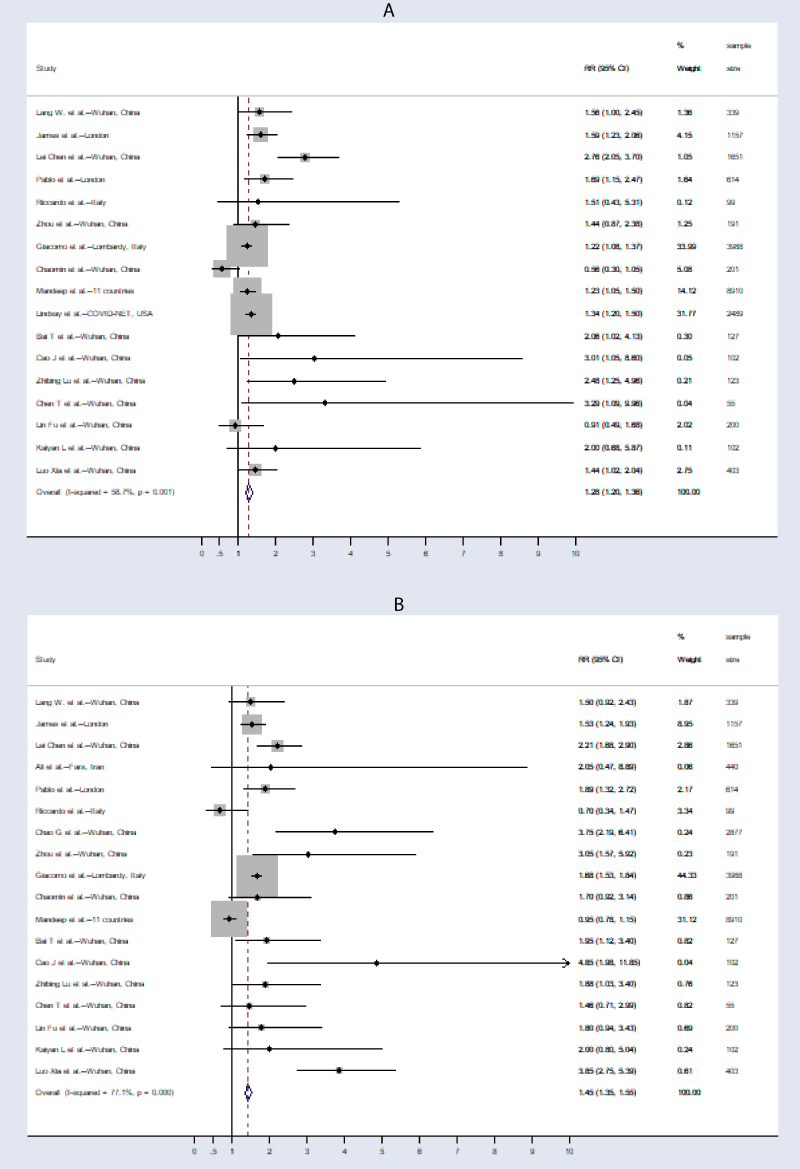
Association between male and mortality of COVID-19 outcome
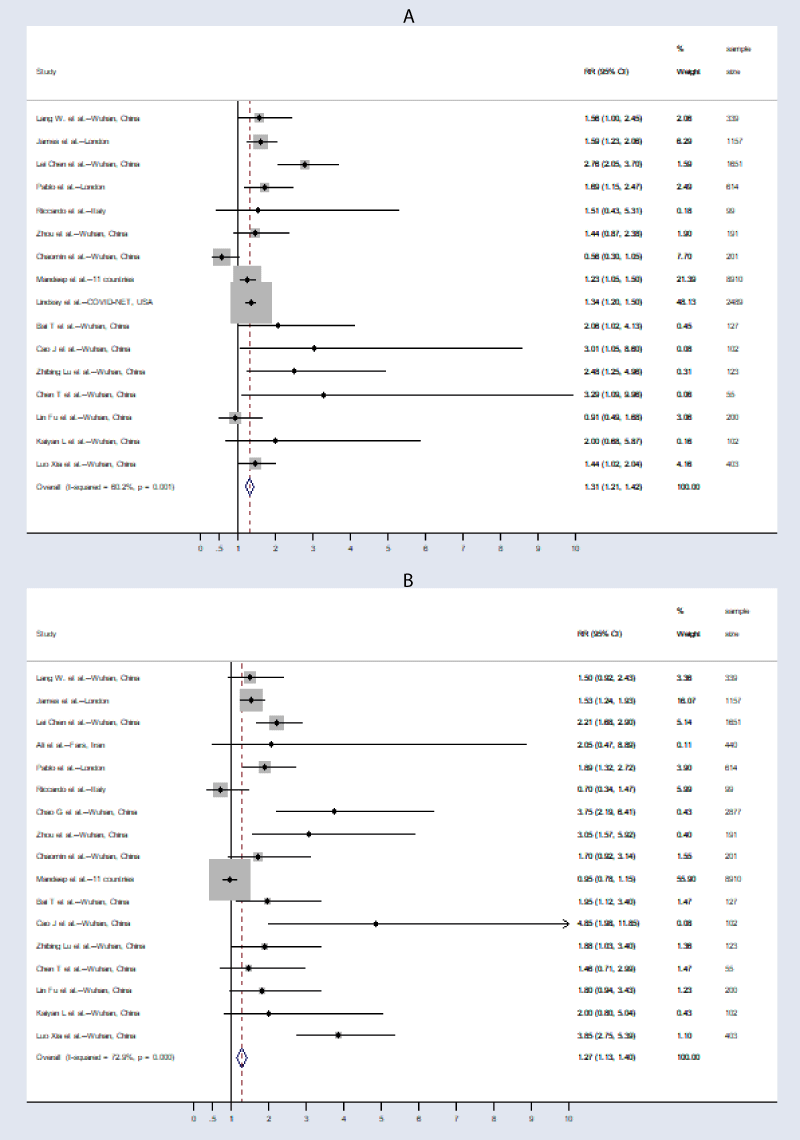
The meta-analysis showed that male patients had a higher mortality due toCOVID-19 infection compared to that with female patients (“RR = 1.28, [95% CI: 1.20-1.36]; I2 = 58.7%, p - value = 0.001”) (Figure 2A). In the leave-one-out sensitivity analysis, we observed that elimination of the highest weight (Giacomo, et al.) study could not change the heterogeneity and the magnitude of association (“RR = 1.31, [95% CI: 1.21 - 1.42]; I2 = 60.2%, p - value = 0.001”) (Figure 3A). The association between being male and mortality was not affected by age (p - value = 0.199) in the meta-regression.
Association between hypertension and mortality of COVID-19 outcome
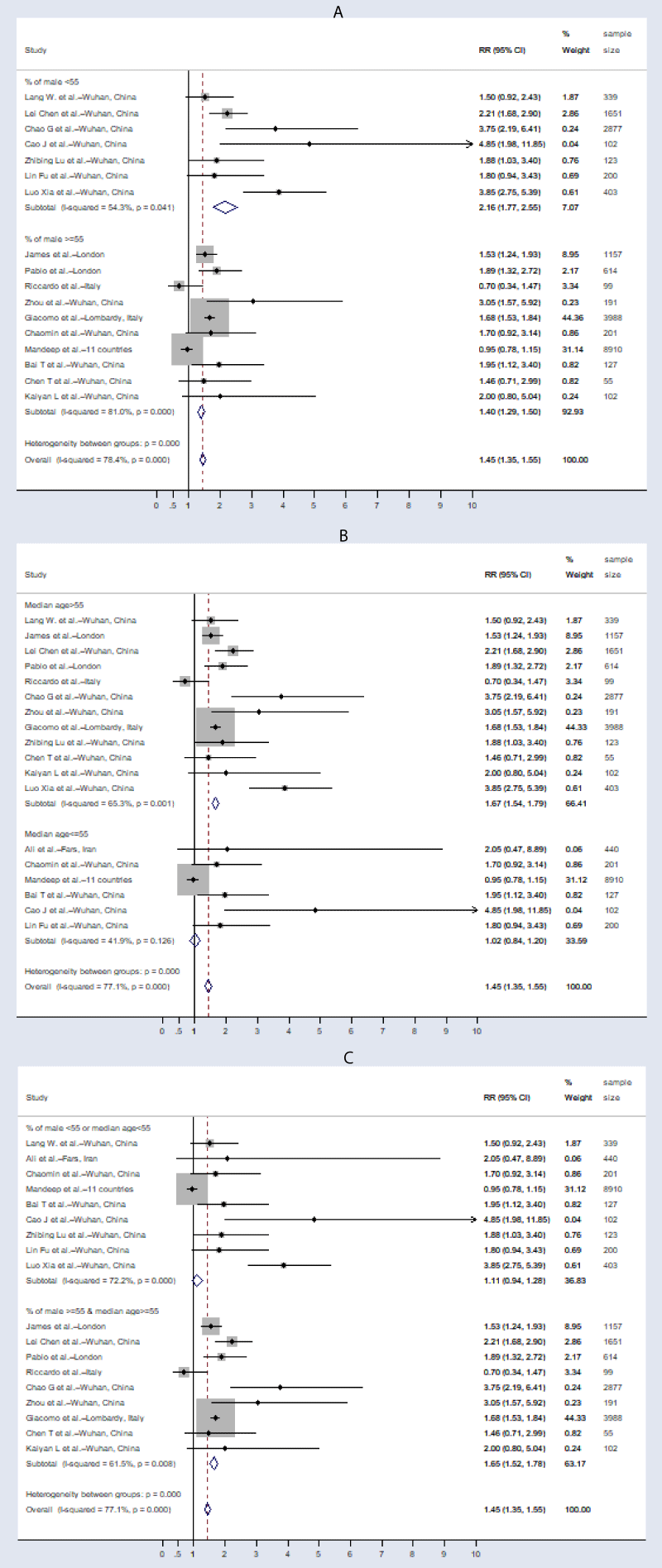
Hypertensive patients with COVID-19 infection were found to be at higher risk of mortality compared to non-hypertensive patients (“RR = 1.45, [95% CI: 1.35 - 1.55]; I2 = 77.1%, p – value < 0.001”) (Figure 2B). In the leave-one-out sensitivity analysis, the elimination of highest weight (Giacomo, et al.) study slightly reduced the magnitude of the association (“RR = 1.27, [95% CI: 1.13 - 1.40]; I2 = 72.9%, p - value < 0.001”) (Figure 3B). The association between hypertension and mortality was affected by sex (p = 0.049), but not age (p = 0.301) and diabetes mellitus (p = 0.343) in the meta-regression analysis. The studies with male ≥ 55% and median age ≥ 55 years (“RR = 1.65, [95% CI: 1.52 - 1.78]; I2 = 77.1%, p – value < 0.001”) had significantly higher association compared to those of studies with male < 55% or median age < 55 years “(RR = 1.11, [95% CI: 0.94 - 1.28]; I2 = 72.2%, p – value < 0.001”) (Figure 4) in the subgroup analysis.
Figure 2: Forest plot for (A) male and mortality of COVID-19 disease; (B) hypertension and mortality of COVID-19 disease: plots show that male and hypertension were associated with mortality with COVID-19 outcome.
Figure 3: Sensitivity analysis: Removal Giacomo, et al. study reduces association between hypertension and mortality but not the association between male and mortality with COVID-19 outcome.
Figure 4: Sub-group analysis showed the association between hypertension and mortality was stronger in studies with (A) single male < 55% (B) single median age > 55 years and (C) combined with male ≥ 55% and age ≥ 55 years.
Publication bias
We found a qualitatively symmetrical association with mortality and other factors (male and hypertension) in the funnel-plot analysis (Figure 5). A further Regression-based Egger’s test showed that there was no effect of a small study on the association with mortality and other factors (male: p - value = 0.138; hypertension: p –value = 0.290).
Figure 5: Funnel plot analysis showed a qualitatively symmetrical funnel plot for the association between mortality and (A) male, and (B) hypertension.
In this systematic review and meta-analysis study, we observed that hypertension were associated with the increased risk of mortality in COVID-19 infections. Meta-regression showed that the association between hypertension and mortality was influenced by sex, which was addressed by the previous severe COVID-19 outcome studies[15]. Further subgroup analysis showed a significantly stronger association in the studies with a higher proportion of male and elderly patients, which is steady with severe and fatal patients in the prior analysis [16].
Although the association between sex and mortality was weaker in the five studies [17–21], meta-analysis shows that the male COVID-19 infected patients were 1.28 times more likely to die. Even though the proportion of male patients was higher (58.8%) than the female patients in the present studies, a male patient had increased risk of dying independent of age. We found similar results with severely infected patients in studies from China [22,23]. The mean score of all comorbidities in men (3.1) was significantly higher than women (1.8) (p - value < 0.05) [24] while the prevalence of hypertension is 25% in men and 20% in women worldwide [7]. However, the COVID-19 infected male patients had more risk of dying than the female patients probably due to weaker immune function in males with existence chronic condition [25–28].
The hypertensive patients were more likely to have a fatal COVID-19 infection compared to non-hypertensive patients in the present study. It is consistent with the prior studies which illustrated that hypertension causes death among COVID-19 patients [6,15,16]. However, the hypertensive patients were more adversely affected by SARS-CoV-2 virus that enters the epithelial cells passing through angiotensin-converting enzyme 2(ACE2). ACE2 decreases vascular inflammatory action of angiotensin 1-7 [29,30]. Inflammatory storm in infected patients releases cytokines causes systemic immune function damage, which may be a significant cause of multiple organ failure and even death [31].
Subgroup analysis showed that the increased mortality with COVID-19 disease was more significant in a higher proportion of male > 55 years with hypertensive patient studies. However, sex and age were more explained in the association between mortality of COVID-19 outcome and hypertension because circulating protein expression of ACE2 is higher in older men with hypertensive condition [8,32].
This study has several limitations. Since angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II type 1 receptor blockers (ARBs) treatment are used in COVID-19 patients with hypertension, it may affect the outcome. Data on hypertensive medicine or therapy were not included in the selected studies. Almost all of the studies were retrospective and peer-reviewed, however, a few preprints before peer review were also included in the meta-analysis. Included studies were from Asia, Europe and North America, however, most of the studies were from China but from different hospitals, therefore, the sample might not represent COVID-19 patients globally.
In conclusion, hypertensive patients are strongly associated with higher odds of mortality due to COVID-19 infections which may account for the contradiction in the many studies. The effect of coexistence hypertension on the risk of mortality with COVID-19 patients was more influential in elderly male patients. We should direct more attention to COVID-19 and hypertensive patients, especially in elderly men in the course of treatment to reduce mortality. Further, more comprehensive studies are needed to investigate more detailed information on the association between hypertension and death of COVID-19 patients, particularly in low-middle income countries.
- Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Eurosurveillance. 2020; 25: 2000058. PubMed: https://pubmed.ncbi.nlm.nih.gov/32019669/
- World Health Organization (WHO). WHO announces COVID-19 outbreak a pandemic. 2020; https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic
- WHO Western Pacific, World Health Organization. 2020. https://www.who.int/westernpacific/emergencies/covid-19
- Worldometers.info Coronavirus Update (Live). 2020. https://www.worldometers.info/coronavirus/
- World Health Organization (WHO). Non communicable diseases. 2020. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020; 101623
- World Health Organization (WHO). Hypertension. 2020. https://www.who.int/news-room/fact-sheets/detail/hypertension
- Lionakis N, Mendrinos D, Sanidas E, Favatas G, Georgopoulou M. Hypertension in the elderly. World J Cardiol. 2012; 4: 135-147. Lionakis N, Mendrinos D, Sanidas E, Favatas G, Georgopoulou M. Hypertension in the elderly. World J Cardiol. 2012; 4: 135.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003; 289: 2560–2571. PubMed: https://pubmed.ncbi.nlm.nih.gov/12748199/
- Klein S, Pekosz A, Passaretti C, Anker M, Olukoya P. Sex, gender and influenza. Geneva World Health Organ. 2010; 1–58.
- vom Steeg LG, Klein SL. SeXX matters in infectious disease pathogenesis. PLoS Pathog. 2016; 12: e1005374. PubMed: https://pubmed.ncbi.nlm.nih.gov/26891052/
- Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016; 16: 626-638. Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016; 16: 626. PubMed: https://pubmed.ncbi.nlm.nih.gov/27546235/
- Roved J, Westerdahl H, Hasselquist D. Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences. Horm Behav. 2017; 88: 95–105. PubMed: https://pubmed.ncbi.nlm.nih.gov/27956226/
- Fleming PS, Koletsi D, Pandis N. Blinded by PRISMA: are systematic reviewers focusing on PRISMA and ignoring other guidelines? PLoS One. 2014; 9: e96407. PubMed: https://pubmed.ncbi.nlm.nih.gov/24788774/
- Pranata R, Lim MA, Huang I, Raharjo SB, Lukito AA. Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression. J Renin-Angiotensin-Aldosterone Syst. 2020; 21: 1470320320926899. PubMed: https://pubmed.ncbi.nlm.nih.gov/32408793/
- Lippi G, Wong J, Henry BM. Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med. 2020; 130: 304–309. PubMed: https://pubmed.ncbi.nlm.nih.gov/32231171/
- Inciardi RM, Adamo M, Lupi L, Cani DS, Di Pasquale M, et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020; 41: 1821–1829. PubMed: https://pubmed.ncbi.nlm.nih.gov/32383763/
- Zhou F, Yu T, Du R, Fan G, Liu Y, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395: 1054-1062. PubMed: https://pubmed.ncbi.nlm.nih.gov/32171076/
- Wu C, Chen X, Cai Y, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180: 934-943. PubMed: https://pubmed.ncbi.nlm.nih.gov/32167524/
- Fu L, Fei J, Xiang HX, Xiang Y, Tan ZX, et al. Analysis of death risk factors among 200 COVID-19 patients in Wuhan, China: a hospital-based case-cohort study. Fang-Fang Liu Hong-Yan Zheng Ling Li Ying Zhao Hui Xu -Xiang Anal Death Risk Factors Among.2020; 200.
- Li K, Chen D, Chen S, Feng Y, Chang C, et al. Radiographic findings and other predictors in adults with Covid-19. MedRxiv. 2020.
- Jin JM, Bai P, He W, Wu F, Liu XF, et al. Gender differences in patients with COVID-19: Focus on severity and mortality. Front Public Health. 2020; 8: 152. PubMed:https://pubmed.ncbi.nlm.nih.gov/32411652/
- Zhang J, Dong X, Cao Y, Yuan Y, Yang Y, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. 2020; 75: 1730-1741. PubMed: https://pubmed.ncbi.nlm.nih.gov/32077115/
- Almagro P, García FL, Cabrera F, Montero L, Morchón D, et al. Grupo Epoc De La Sociedad Española De Medicina Interna Comorbidity and gender-related differences in patients hospitalized for COPD. The ECCO study. Respir Med. 2010; 104: 253–259. PubMed: https://pubmed.ncbi.nlm.nih.gov/19879744/
- Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016; 49: 129–133. PubMed: https://pubmed.ncbi.nlm.nih.gov/27352628/
- Jaillon S, Berthenet K, Garlanda C. Sexual dimorphism in innate immunity. Clin Rev Allergy Immunol. 2019; 56: 308-321. PubMed: https://pubmed.ncbi.nlm.nih.gov/28963611/
- Channappanavar R, Fett C, Mack M, Ten Eyck PP, et al. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017; 198: 4046–4053. PubMed: https://pubmed.ncbi.nlm.nih.gov/28373583/
- Dryden M, Baguneid M, Eckmann C, Corman S, Stephens J, et al. Pathophysiology and burden of infection in patients with diabetes mellitus and peripheral vascular disease: focus on skin and soft-tissue infections. Clin Microbiol Infect. 2015; 21: S27–S32. PubMed: https://pubmed.ncbi.nlm.nih.gov/26198368/
- Schiffrin EL, Flack JM, Ito S, Muntner P, Webb RC. Hypertension and COVID-19. Am J Hypertens. 2020; 33: 373–374. PubMed: https://pubmed.ncbi.nlm.nih.gov/32251498/
- Guo J, Huang Z, Lin L, Lv J. Coronavirus Disease 2019 (COVID‐19) and Cardiovascular Disease: A Viewpoint on the Potential Influence of Angiotensin‐Converting Enzyme Inhibitors/Angiotensin Receptor Blockers on Onset and Severity of Severe Acute Respiratory Syndrome Coronavirus 2 Infection. J Am Heart Assoc. 2020; 9: e016219. PubMed: https://pubmed.ncbi.nlm.nih.gov/32233755/
- Rossi GP, Sanga V, Barton M. Potential harmful effects of discontinuing ACE-inhibitors and ARBs in COVID-19 patients. eLife. 2020; 9: e57278. PubMed: https://pubmed.ncbi.nlm.nih.gov/32250244/
- Chen T, Dai Z, Mo P, Li X, Ma Z, et al. Clinical Characteristics and Outcomes of Older Patients with Coronavirus Disease 2019 (COVID-19) in Wuhan, China: A Single-Centered, Retrospective Study. J Gerontol A Biol Sci Med Sci. 2020; 75: 1788-1795. PubMed: https://pubmed.ncbi.nlm.nih.gov/32279081/